HEALTHCARE OPERATIONS WORKSHOP 2023
The program is finalized! Please see below.
Click here for program detail and abstracts
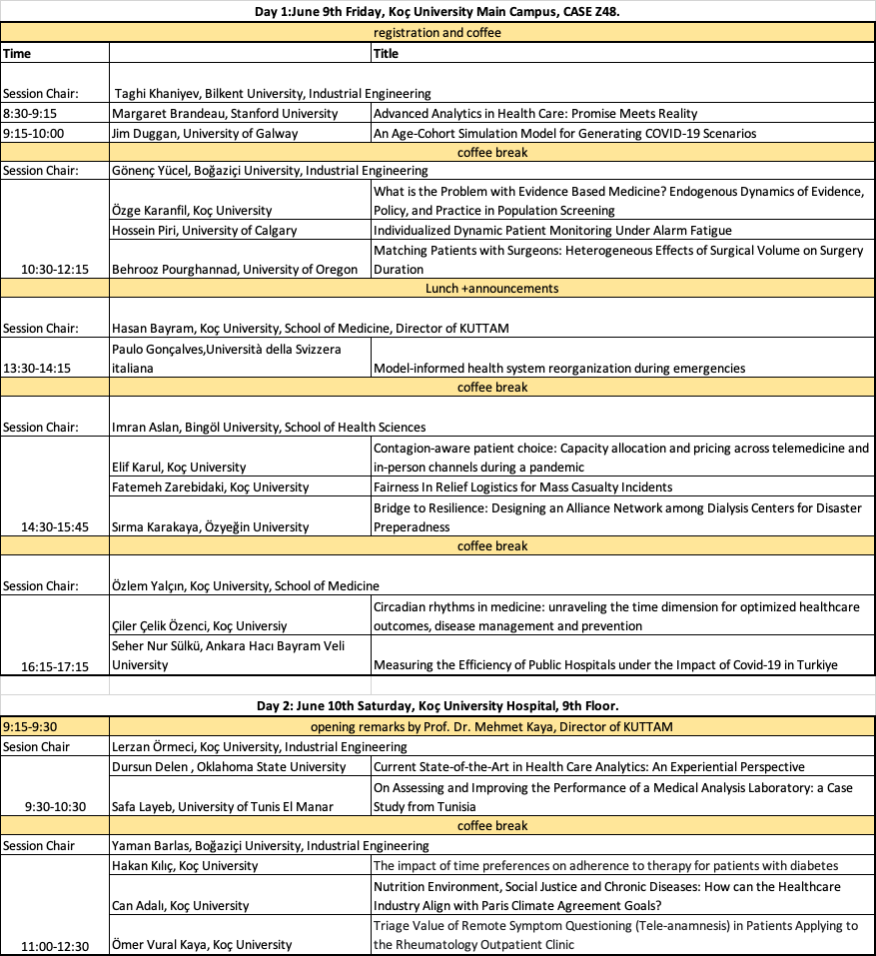
| Day 1:June 9th Friday, Koç University Main Campus, CASE Z48. | ||
| registration and coffee | ||
| Time | Title | |
| Session Chair: | Taghi Khaniyev, Bilkent University, Industrial Engineering | |
| 8:30-9:15 | Margaret Brandeau, Stanford University | Advanced Analytics in Health Care: Promise Meets Reality |
| 9:15-10:00 | Jim Duggan, University of Galway | An Age-Cohort Simulation Model for Generating COVID-19 Scenarios |
| coffee break | ||
| Session Chair: | Gönenç Yücel, Boğaziçi University, Industrial Engineering | |
| 10:30-12:15 | Özge Karanfil, Koç University | What is the Problem with Evidence Based Medicine? Endogenous Dynamics of Evidence, Policy, and Practice in Population Screening |
| Hossein Piri, University of Calgary | Individualized Dynamic Patient Monitoring Under Alarm Fatigue | |
| Behrooz Pourghannad, University of Oregon | Matching Patients with Surgeons: Heterogeneous Effects of Surgical Volume on Surgery Duration | |
| Lunch +announcements | ||
| Session Chair: | Hasan Bayram, Koç University, School of Medicine, Director of KUTTAM | |
| 13:30-14:15 | Paulo Gonçalves,Università della Svizzera italiana | Model-informed health system reorganization during emergencies |
| coffee break | ||
| Session Chair: | Imran Aslan, Bingöl University, School of Health Sciences | |
| 14:30-15:45 | Elif Karul, Koç University | Contagion-aware patient choice: Capacity allocation and pricing across telemedicine and in-person channels during a pandemic |
| Fatemeh Zarebidaki, Koç University | Fairness In Relief Logistics for Mass Casualty Incidents | |
| Sırma Karakaya, Özyeğin University | Bridge to Resilience: Designing an Alliance Network among Dialysis Centers for Disaster Preperadness | |
| coffee break | ||
| Session Chair: | Özlem Yalçın, Koç University, School of Medicine | |
| 16:15-17:15 | Çiler Çelik Özenci, Koç Universiy | Circadian rhythms in medicine: unraveling the time dimension for optimized healthcare outcomes, disease management and prevention |
| Seher Nur Sülkü, Ankara Hacı Bayram Veli University | Measuring the Efficiency of Public Hospitals under the Impact of Covid-19 in Turkiye | |
| Day 2: June 10th Saturday, Koç University Hospital, 9th Floor. | ||
| 9:15-9:30 | opening remarks by Prof. Dr. Mehmet Kaya, Director of KUTTAM | |
| Sesion Chair | Lerzan Örmeci, Koç University, Industrial Engineering | |
| 9:30-10:30 | Dursun Delen , Oklahoma State University | Current State-of-the-Art in Health Care Analytics: An Experiential Perspective |
| Safa Layeb, University of Tunis El Manar | On Assessing and Improving the Performance of a Medical Analysis Laboratory: a Case Study from Tunisia | |
| coffee break | ||
| Session Chair | Yaman Barlas, Boğaziçi University, Industrial Engineering | |
| 11:00-12:30 | Hakan Kılıç, Koç University | The impact of time preferences on adherence to therapy for patients with diabetes |
| Can Adalı, Koç University | Nutrition Environment, Social Justice and Chronic Diseases: How can the Healthcare Industry Align with Paris Climate Agreement Goals? | |
| Ömer Vural Kaya, Koç University | Triage Value of Remote Symptom Questioning (Tele-anamnesis) in Patients Applying to the Rheumatology Outpatient Clinic | |
Koç University Healthcare Operations Workshop 2023
Abstracts
DAY 1:
Session 1: 8:30-10:00
Advanced Analytics in Health Care: Promise Meets Reality
Margaret Brandeau
Advanced analytic techniques such as artificial intelligence (AI), have great potential to transform many aspects of health care – but despite this promise have only been implemented in a limited number of settings and in a limited way. This talk begins by discussing the potential of AI and advanced analytics to transform health care in areas such as disease diagnosis and treatment, disease monitoring, patient monitoring and clinical outcome prediction, health care operations, and health care administration. We then outline the many reasons why this potential has not been realized. As a microcosm illustrating the state of AI and advanced analytics applications, we describe a number of projects carried out at Lucile Packard Hospital Stanford. We conclude with thoughts about what is needed in order for AI to be successfully integrated into health care systems and the next steps that can be taken to advance implementation.
An Age-Cohort Simulation Model for Generating COVID-19 Scenarios
Jim Duggan
The COVID-19 pandemic presented an immediate need for the Irish Government to establish modelling capacity to inform public health decision making. A broad-based interdisciplinary team was created at short notice, drawing together related expertise from the academic and health sectors. This presentation documents one of a number of modelling solutions developed by the Irish Epidemiological Modelling Advisory Group (IEMAG), which advised the Irish Government on COVID-19 responses during the pandemic. This solution deployed a modular simulation design, with three benefits: (1) it enabled a simplification of the disease transmission structure; (2) it provided a practical workflow to coordinate activities; and (3) it speeded up the process of scenario generation and the requirement to provide timely and informative, scenario analysis to support Ireland’s pandemic response. An example provides an insight into the model outputs and scenarios generated as the Omicron wave was taking hold in Ireland in early December 2021, and overall conclusions and lessons learned are discussed.
Session 2: 10:30-12:15
What is the Problem with Evidence Based Medicine? Endogenous Dynamics of Evidence, Policy, and Practice in Population Screening
Özge Karanfil
Clinical practice guidelines (CPGs) for routine screening and treatment are contentious and often change over time. Some tests are over- or underused, with clinical practice persistently deviating from evidence. While there is a proliferation of modeling studies to inform CPGs, not many are addressing the actual guideline-making process itself. We develop an integrated, broad boundary feedback theory and a series of formal simulation models to investigate the universal problem of evidence-based development of sound and reliable guidelines. We continue with an extended case study for prostate cancer screening to explain why some tests are over- while others are underused, contrary to available scientific evidence. Long-term trends in population screening and other related problems (significant variations, over- and underuse, gaps between evidence, policy, and practice, suboptimality and fluctuations in guidelines) are discussed with overall conclusions within the context of developed and developing countries, and in repeated managerial contexts.
Individualized Dynamic Patient Monitoring Under Alarm Fatigue
Hossein Piri
Steven Shechter, Tim Huh, Darren Hudson
Hospitals are rife with alarms, many of which are false. This leads to alarm fatigue, in which clinicians become desensitized and may inadvertently ignore real threats. We develop a partially observable Markov decision process model for recommending dynamic, patient-specific alarms in which we incorporate a cry-wolf feedback loop of repeated false alarms. Our model takes into account patient heterogeneity in safety limits for vital signs and learns a patient’s safety limits by performing Bayesian updates during a patient’s hospital stay. We develop structural results of the optimal policy and perform a numerical case study based on clinical data from an intensive care unit. We find that compared with current approaches of setting patients’ alarms, our dynamic patient-centered model significantly reduces the risk of patient harm.
Matching Patients with Surgeons: Heterogeneous Effects of Surgical Volume on Surgery Duration
Behrooz Pourghannad
Guihua Wang
We study how patient-specific information can be leveraged to improve a hospital’s operational efficiency. We develop a framework to utilize patient-specific information by addressing three important questions: (1) Is the effect of surgical volume heterogeneous across patients with different features? (2) If so, how does one generate patient-specific information that captures the heterogeneous effects of surgical volume on surgery duration? (3) What is the value of patient-specific information in helping a hospital improve its operational efficiency? We use a novel machine learning approach, i.e. causal forest, to obtain patient-specific volume effects. We provide empirical evidence that the effect of surgical volume is heterogeneous and address the challenges of estimating heterogeneous effects for different patients. Finally, we use patient-specific volume effects and an optimization model to assess the potential value of patient-specific information in improving a hospital’s operational efficiency. We find the total duration of surgeries could be reduced by 3\% to 18\% if patient-specific volume effects are taken into account. Our framework is valuable to hospital administrators because it improves a hospital’s operational efficiency by using patient-specific volume effects to match patients with surgeons. Full paper link: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3699215
Session 3:13:30-14:15
Model-informed health system reorganization during emergencies
Paulo Gonçalves
Problem definition: This paper describes the real-time participatory modeling work that our team of
academics, public health officials, and clinical decision makers has been undertaking to support the regional efforts to tackle COVID-19 in the East of England (EoE). Methodology: Since March 2020, we have been studying research questions that have allowed us to address the pandemic’s rapidly evolving current and near-future epidemiological state, as well as short-term (a few weeks) and medium-term (several months) bed capacity demand. Frequent data input from and consultations with our public health and clinical partners allow our academic team to apply dynamic data-driven approaches using time series modeling and system dynamics modeling. We thus obtain a broad view of the evolving situation. Results: The academic team presents the model outcomes and insights during weekly joint meetings among public health services, national health services, and other academics to support COVID-19 planning activities in the EoE, contributing to the discussion of the COVID-19 response and issues beyond immediate COVID-19 planning. Academic/practical relevance: As COVID-19 planning efforts necessitate a rapid response, our short-and medium-term forecasting models aim to achieve the right balance between rigor and speed in the face of an uncertain and constantly changing situation. Managerial implications: Our regional and local focus enables us to better understand the pandemic’s progression and to help decision makers make more informed short- and medium-term capacity plans in different localities in the EoE. In addition, the knowledge gained through our collaborative experiences may inform guidance on how academics and practitioners can successfully collaborate in rapid response to disasters such as COVID-19.
Session 4: 14:30-15:45
Contagion-aware patient choice: Capacity allocation and pricing across telemedicine and in-person channels during a pandemic
Elif Karul
Erhun Özkan, Zeynep Akşin
Driven by the fear of contagion during the Covid-19 pandemic, patient demand has shifted, resulting in increased demand for telemedicine service as well as avoidance of medical care. We propose a demand model with endogenous contagion-aware patient choices between no appointment, telemedicine and in-person appointments, where choices drive volume which in turn drives contagion. First, we study optimal capacity allocation for these services to maximize a healthcare center’s revenue under given prices. We show that when the capacity is abundant and as the volume of patients increases, the number of patients choosing in-person appointments increases at a much slower rate than the number of patients choosing telemedicine appointments does. This leads to a significant revenue loss and underlines the importance of the telemedicine channel as a major source of revenue when there is fear of contagion. Second, we show that the optimal pricing strategy leads to a higher price for the in-person appointments under equal coinsurance. Finally, we incorporate the concurrent possibility of physician infection in the model, captured by a decrease in the healthcare center’s effective capacity as a function of in-person volume. In this setting, we compare the outcomes of revenue maximization with social welfare maximization. We show that relative to revenue maximization, maximizing social welfare allocates more capacity and assigns a lower price for the telemedicine channel, decreasing the number of infected physicians.
Fairness In Relief Logistics for Mass Casualty Incidents
Fatemeh Zarebidaki
In recent years, there have been numerous large-scale incidents, terrorist attacks, and natural disasters. Consequently, emergency operations management must be developed to maximize survivability and minimize victims’ distress while maintaining fairness in the provision of humanitarian aid. In the aftermath of a mass casualty event, triage systems evaluate victims’ health conditions and prioritize their transport to hospitals based on severity. Typically, the order of service to victims is determined solely by categorizing the casualties, regardless of the availability of resources or the severity of the crisis. In some instances, victims lose their lives because of delays in treatment. This study’s mathematical model incorporates triage considerations (survival probabilities), transportation resource limitations, and victims’ distress into decision making and demonstrates the influence of equity consideration on the success of rescue attempts. In our model, which is an application of the Capacitated vehicle routing problem with time windows (CVRPTW), we aggregate various versions of VRP features to address capacity, deadlines, victims’ distress, and fairness concerns. Regarding the emergency nature of the decision-making process, both time constraints and rescue team expectations should be considered. Therefore, we employ two heuristic methods based on swarm intelligence (Ant colony system optimization variants and Artificial bee colony) to provide nearly optimal solutions in a reasonable amount of time. In sum, this study brings previously recognized limits into crisis management and aims to reduce calculation time in emergency relief to match rescue teams’ expectations.
Bridge to Resilience: Designing an Alliance Network among Dialysis Centers for Disaster Preparedness
Sırma Karakaya
Burcu Balçık, Evrim Güneş
Dialysis treatment is a continuous treatment plan, where patients must receive the treatment three times per week for long years. Any interruption in treatment can lead to fatal consequences, making it crucial to ensure that dialysis clinic networks are resilient to potential disasters that may render the clinics inoperable. To address this problem, we build an alliance network among dialysis clinics, allowing clinics to share their available resources in the aftermath of a disaster. We assign each patient a number of back-up centers among the clinics that the pre-disaster clinics of patients have formed alliances with. The aim of the alliance network problem (ANP) is to minimize the expected treatment cost of the dialysis patients. The ideal situation for a patient is to continue receiving treatment in its pre-disaster clinic. If it is not possible, the second-best option is to receive treatment in one of the assigned backup centers. This option can reduce delays in treatment and improve patient outcomes, as the pre-disaster clinic and backup center work in alliance and can coordinate the transfer of patients and medical records. If none of the back-up centers are available, the third option is to assign patients to other clinics within the network. Although patients may experience delays in finding an available clinic, they can still receive treatment. The worst scenario is when patients cannot be assigned to any clinics. In this case, patients may face prolonged treatment interruptions, leading to life-threatening conditions. In the scope of this study, we evaluate various alliance sizes and structures. Using the data of the dialysis centers located on the Anatolian side of Istanbul we aim to propose practically applicable alliance configurations and enhance resilience to mitigate the risks posed by possible disasters. By analyzing and optimizing alliance networks, our findings can contribute to improving post-disaster dialysis treatment continuity and patient outcomes.
Session 5: 16:15-17:15
Circadian rhythms in medicine: unraveling the time dimension for optimized healthcare outcomes, disease management and prevention
Çiler Çelik Özenci
Circadian rhythms (CRs), the endogenous biological oscillations that occur approximately every 24 hours, are integral to human health. While physicians typically diagnose and treat diseases without considering temporality, time may be a critical factor in medical practice. A growing body of evidence shows that molecular clocks regulate 24-hour CRs in vital cardio-metabolic, endocrine, immunological, and behavioral processes. In addition, a growing number of studies indicate a link between circadian rhythm disruption (CRD), common in modern, always-on societies, and the prevalence, severity, and progression of several non-communicable diseases, including cancer, cardiovascular disease, and mental disorders. In addition, maternal chronodisruption has been associated with intrauterine growth restriction (IUGR). IUGR infants, who account for 3-7% of all births worldwide and 24% of newborns in developing countries, are predisposed to non-communicable diseases (NCDs) in adulthood, such as cardiovascular disease, hypertension, metabolic syndrome, and behavioral problems, in line with the Developmental Origins of Health and Disease (DOHaD) hypothesis, with significant societal implications. Circadian medicine aims to incorporate knowledge of 24-hour biological rhythms not only to optimize diagnostic and therapeutic strategies focusing on drug delivery, disease management, and overall patient well-being but also to prevent circadian-related disorders. The potential for integrating chronobiology into clinical practice begins with a deeper understanding of CRs and their impact on human health and disease, ultimately enabling more personalized healthcare, improved patient outcomes, and reduced healthcare costs. This burgeoning field of medicine promises the significant potential to improve disease prevention, diagnosis, and treatment, benefiting patients and healthcare systems alike.
MEASURING EFFICIENCY of PUBLIC HOSPITALS UNDER the IMPACT of COVID-19 in TÜRKİYE
Seher Nur Sülkü
Alper Mortaş, Aziz Küçük
The Covid-19 pandemic has had serious medical, administrative and financial effects on the health system and hospitals around the world. In Türkiye, compared to 2019 realizations, in 2020 and 2021 respectively there were 39% and 21% decrease in the number of outpatient services and 29% and 17% decline in total inpatient services of public hospitals. The main subject of this research is how the pandemic period affects the Turkish public hospitals’ efficiency. We have measured the technical efficiency of outpatient and inpatient care services of Turkish public hospitals using Stochastic Frontier Analysis (SFA). The dataset includes 563 hospitals for the years 2015 through 2021. Inputs of number of physicians, nurses and other medical staff, and number of beds and their interactions with each other are introduced to the SFA models of outputs of outpatient visits and inpatient discharges adjusted with case mix index are derived. Firstly, we found that the years associated with Covid-19 have a significant negative impact on the inpatient service efficiency. Training and Research and City Hospitals have low efficiency scores in outpatient services but high efficiency scores in inpatient services. In addition, the regions with high population rates have positive impact in outpatient efficiency and negative impact in inpatient efficiency. During the pandemic, city hospitals, have received large investments, gained a key role by increasing both the patient load and their efficiency. Future reforms can be guided by taking advantage of the efficiency differences of hospitals in different environmental factors.
DAY 2:
Session 1: 9:30-10:30
Current State-of-the-Art in Health Care Analytics: An Experiential Perspective
Dursun Delen
Data analytics, big data, data science, and AI/machine learning—relatively new buzzwords—are gaining popularity in every facet of businesses and sciences around the world like nothing else that we have witnessed in recent history. Their attractiveness is particularly notable in the field of healthcare and medicine, often called Health Analytics. A strong testament to the potential of health analytics is the increasing emphasis given to this field by the major funding agencies in the U.S. For instance, the National Institute of Health (NIH) and the National Science Foundation (NSF) collaboratively created a series of multi-million-dollar funding opportunities under the name of “Smart and Connected Heath.” The main reasons for this popular adoption of analytics in health care include: • Need – increasing demand coupled with decreasing resources forcing healthcare organizations to do more with less (i.e., be effective and efficient at the same time). • Technology availability – software/algorithms are becoming more sophisticated while simultaneously the hardware and infrastructure continue to be better, faster, and less expensive. • Data availability – data is ubiquitous. As the saying goes “we are drowning in data but starving for knowledge.” Organizations that are effective in converting data into information and knowledge are those most likely to survive and thrive in these difficult economic conditions. • Cultural shift – the reliance on data-driven, fact-based actionable information is becoming more prevalent in health care. The sole reliance on experience and intuition is finally giving way to data and analytics in decision-making processes. This presentation will offer a broad experiential perspective on the current and future trends in health analytics and will provide exemplary research projects to further motivate the increasing popularity of the field.
On Assessing and Improving the Performance of a Medical Analysis Laboratory: a Case Study from Tunisia
Safa Bhar Layeb
Mohamed Yassine Kaabar, Imen Mejri, Najla Aissaoui
To provide high-quality care efficiently, healthcare decision-makers are focused on measuring and improving their performance due to increased demand, rising costs, and limited resources. In this context, this study was conducted by an interdisciplinary team within a medical analysis laboratory of a Tunisian university hospital. More than 50 000 samples are collected per year, under the responsibility of medical biologists. The objective is to analyze the current situation in order to propose concrete solutions that could be easily transposed to effectively meet the needs of all the stakeholders. Toward this end, three major work projects have been carried out. In the first project, we were interested in assessing the satisfaction of patients as well as prescribers. Both of them express increasing claims regarding the accessibility to health care while requiring quality guarantees. For that purpose, we have proposed and conducted punctual and easily reproducible satisfaction surveys that simultaneously involve the two aforementioned stakeholders. The collected data were then screened by several descriptive and analytical statistical analysis tools, such as principal component analysis, using R software. Numerical experiments have identified the strengths as well as the weaknesses of the laboratory that lead to the dissatisfaction of patients and prescribers. The second project have tackled the organizational issues of the laboratory in order to minimize the cycle time of the patients’ pathway and improve its service performance. After having modeled the outpatients’ process, we proposed a simulation model. This modeling step is the core of Discrete Event Simulation using the ARENA software. In fact, such an approach finds its interest in investigating patients’ flows with stochastic aspects and testing the impact of a change made on several parameters. Several improvement scenarios were derived and assessed based on their impact on the patients’ waiting time and length of stay within the laboratory department. The objective of the third work project was the optimization of the inventory management system for reagents and consumables in the laboratory. Therefore, we have begun by modeling and analyzing the current supply processes of reagents and consumables using Business Process Model and Notation and Ishikawa diagrams. The current state was assessed using the collected corresponding data. Besides, this has allowed the identification of the main deficiencies leading to poor inventory management. Precisely, these defects are on the level of the layout, the organization of storage areas, the misuse of the Decision Support System (DSS), and the poor estimation of annual quantities to order. Thus, we have contributed to the implementation of the recent DSS and the accompaniment of the laboratory staff to its use. In fact, the transition from manual to computerized inventory management was a radical change for most of the staff, and for this reason, several changes must be carried out in order to adapt this transition to the laboratory environment. In order to conduct this change, the ADKAR methodology was adopted. Furthermore, we have focused on the organization and utilization of the storage areas. We were interested in finding concrete solutions for the sizing of the stock and for the traceability of the movements of stock out. To go further in reducing shortages and overstock risks, we have developed a well-engineered framework for demand forecasting. The conducted actions have led to a substantial increase in laboratory performance.
Session 2: 11:00-12:30
The impact of time preferences on adherence to therapy for patients with diabetes
Hakan Kılıç
Oğuzhan Deyneli, Evrim Güneş, Şeyda Özcan
Non-adherence to therapy for patients with diabetes can cause deterioration of their health. This can lead to hospitalizations that increase costs to the healthcare system. Patient adherence is associated with many factors. One of them is the perceived value of the treatment, which can be affected by how much a patient considers his future, i.e., his time preferences. We empirically examine the impact of time preferences on patient adherence in terms of impatience, procrastination and self-awareness about procrastination. The previous work on this topic presents mixed conclusions about the relationship between adherence and time preferences. Moreover, there is no study investigating the effect of self-awareness. In addition to filling this gap, we aim to establish new insights by considering all dimension of adherence (medication, self-monitoring, follow-up visits, diet, exercise) together with operational factors such as continuity of care and number of physician visits. A retrospective cohort study is conducted with a sample of 369 responses. The time preferences are measured both qualitatively and quantitatively. Preliminary results of the study will be presented.
Nutrition Environment, Social Justice and Chronic Diseases: How can the Healthcare Industry Align with Paris Climate Agreement Goals?
Can Adalı
Climate crisis and ecological collapse are driving the 6th mass extinction of species, threatening human civilization and the lives of millions of both human and non-human individuals. The evidence shows clearly that both climate change and related ecological crises result from human activities in the past few centuries 1 The GDP-growth-based economy paradigm is one of the drivers of the continuous growth of many sectors, which results in excessive resource extraction, GHG emissions, and habitat destruction. With existing government policies, 3.2Co warming is foreseen by the end of the century which does not meet the 1.5Co goal of the Paris Climate Agreement.
The healthcare industry is one such sector that has been growing and is expected to grow by 3.8% per annum until 2040 (No Harm Europe). As a result, its resource use and GHG emissions are expected to rise as well. One major reason for the growth of the healthcare industry is the growing number of chronic patients over the past few decades. In the USA, up to 90% of healthcare spending is related to chronic diseases and dementia2. The evidence shows that chronic diseases are predominantly caused by lifestyle habits and the majority of them are reversible and preventable. Nutrition has a huge influence on the prevalence of chronic diseases and related deaths. The evidence clearly shows that the more unprocessed, whole plant-based foods, and the fewer animal products and processed foods consumed; the less likely to have chronic diseases and less likely to die of chronic diseases. Other lifestyle factors that influence the prevalence of chronic diseases are physical activity, social relationships, sleep, and chronic stress.
A systems model that captures the relationship between healthcare sector emissions, chronic disease prevalence, and nutrition habits is necessary to validate the hypothesis and analyze possible interventions. At the core of the systems model, there are three stock variables: the number of people who follow a plant-based diet, the number of people who follow omnivore diets and the number of chronic patients. Three major influential mechanisms are the GDP growth-based consumerist systems, cultural and psychological aspects of food choices (carnism and veganism), disease management paradigm of the healthcare system.
Ömer Vural Kaya
Nilüfer Alpay Kanıtez
INTRODUCTION
The Rheumatology Department deals with systemic inflammatory diseases, which often lead to musculoskeletal problems. The majority of musculoskeletal issues in the community fall into the non-inflammatory disease group, highlighting the importance of accurate differential diagnosis in numerous patients. The number of rheumatologists is limited, and inappropriate patient referrals can result in the misuse of existing potential. Effective triage of patients is crucial for efficient healthcare services. Triage is not only a problem specific to rheumatology but also a concern for the national healthcare system. The increasing demand has led to a growing problem of workload and mismanagement of resources. The increasing workload and unmet demand can lead to delays in accessing specialist doctors and disruptions in healthcare services.
There is limited literature on the use of remote symptom questioning or digital anamnesis. A study conducted in 2020 with patients diagnosed with diabetes and depression showed that using a system called a digital medical consultation assistant to communicate with patients contributed to efficient use of time, focusing on the complaint, and obtaining quality information. (1) Another study conducted in 2011 utilized a system called ‘Computer-assisted history taking’. The results indicated that computer-assisted history taking allowed healthcare professionals to use their time efficiently and enabled patients to answer specific questions that they may not want to discuss face-to-face. (2)
METHOD
Purpose of our study is to include 300 patients. Patients who have scheduled appointments at the Rheumatology Department of Koç University Hospital will be included in the study, while those who have previously been diagnosed with any rheumatological disease will be excluded. Once an appointment is scheduled for the designated study group through the call center, an electronically prepared “Remote Symptom Questionnaire” will be sent to them via the Hospital Information Management System (HBYS). Technical support will be provided by our hospital’s Information Technology department. This study is referred to as remote symptom questioning (tele-anamnesis). The questionnaire results and the patient’s file information evaluated by the rheumatology physician (demographic data, complaint, duration, and diagnosis) will be recorded and analyzed. After the actual physical examination, the diagnoses will be classified as inflammatory or non-inflammatory diseases, and compared with the questionnaire the patient answered before coming to the hospital. This way, the effectiveness of remote symptom questioning (tele-anamnesis) in terms of triage will be evaluated based on the information provided by patients before their arrival. The non-inflammatory patient group is more relevant to departments such as physical therapy and rehabilitation or orthopedics.
The use of digital health tools (DHT) is increasingly expanding in various fields. When used correctly, DHT is believed to contribute positively to the healthcare system. Developing and effectively utilizing electronic patient questionnaires or patient-based scales, which are one of the DHTs, can provide easier and more accurate triage. Although there have been limited studies with similar objectives in the literature in recent years, no such study has been found in the field of rheumatology. It is believed that our study will be a good starting point for developing an effective remote anamnesis tool and utilizing it for accurate triage in rheumatology patients.
Inclusion Criteria: Adult individuals between the ages of 18 and 75
Patients who have scheduled appointments at the Rheumatology Department of Koç University Hospital
Exclusion Criteria: Patients previously diagnosed with any rheumatological disease
OBJECTIVE
Previous studies have shown that with the increasing presence of technology in our lives and the use of technological tools, the time allocated to patients can be used more efficiently. It was observed that digital anamnesis forms filled out by patients themselves before coming to the hospital had been previously implemented, but there was a lack of survey studies specifically related to diagnosis in rheumatology clinics. The aim was to contribute new data and insights to the literature in this regard, serving as a precursor for future studies on remote symptom questioning in both rheumatology and other departments. The results will be compared to assess the degree of concordance between the survey results and the clinician’s diagnosis in terms of the inflammatory/non-inflammatory categorization. Additionally, after the initiation of diagnosis-specific treatment, the survey form will be filled out again by the patient to obtain information on regression data. Thus, the aim is to determine how helpful the survey study is in patient triage.
References:
1- Geronimo Jimenez , Shilpa Tyagi , Tarig Osman , Pier Spinazze , Rianne van der Kleij , Niels H Chavannes , Josip Car ; Improving the Primary Care Consultation for Diabetes and Depression Through Digital Medical Interview Assistant Systems: Narrative Review
2- Yannis Pappas, Chantelle Anandan, Joseph Liu, Josip Car, Aziz Sheikh, Azeem Majeed; Computer- asissted history-taking systems (CAHTS) in health care: benefits, risks and potential for further development
INVITED SPEAKER BIOGRAPHIES
Margaret L. Brandeau is Coleman F. Fung Professor of Engineering and Professor of Health Policy (by Courtesy) at  Stanford University. Her research focuses on the development of applied mathematical and economic models to support health policy decisions. Her recent work has examined HIV and drug abuse prevention and treatment programs, programs to control the opioid epidemic, and COVID-19 response strategies. She is an INFORMS Fellow. From INFORMS, she has received the Philip McCord Morse Lectureship Award, the President’s Award, the Pierskalla Prize (twice), and the Award for the Advancement of Women in Operations Research and the Management Sciences. At Stanford she has received the Eugene L. Grant Faculty Teaching Award from the School of Engineering and the Graduate Teaching Award from the Department of Management Science and Engineering.
Stanford University. Her research focuses on the development of applied mathematical and economic models to support health policy decisions. Her recent work has examined HIV and drug abuse prevention and treatment programs, programs to control the opioid epidemic, and COVID-19 response strategies. She is an INFORMS Fellow. From INFORMS, she has received the Philip McCord Morse Lectureship Award, the President’s Award, the Pierskalla Prize (twice), and the Award for the Advancement of Women in Operations Research and the Management Sciences. At Stanford she has received the Eugene L. Grant Faculty Teaching Award from the School of Engineering and the Graduate Teaching Award from the Department of Management Science and Engineering.
Prof. Jim Duggan is a Personal Professor at the School of Computer Science, University of Galway. Prof. Duggan has held a range of senior roles, including Head of Department (two terms), Vice-Dean of Research and Graduate Studies, and has served on the Standing Committee and Academic Council. Prof. Duggan is a member of the Ryan Institute, the Data Science Institute, and is a Funded Investigator at the Insight Centre for Data Analytics. Prof. Duggan is a Managing Editor of the System Dynamics Review, and his research interests span simulation, mathematical modelling and data science, with applications in public health. Prof. Duggan is a member of the Irish Epidemiological Modelling Advisory Group (IEMAG), and also a member of the World Health Organisation’s Global Outbreak and Response Network.
Paulo Gonçalves is Professor of Management and Director of the Humanitarian Operations Group at the Università della Svizzera italiana (USI), Switzerland, and Research Fellow at the University of Cambridge  Judge Business School (CJBS). Prior to USI, He was visiting Assistant Professor at MIT Sloan and Assistant Professor at the University of Miami Graduate School of Business. Paulo holds a Ph.D. in Management Science and System Dynamics from MIT Sloan and a M.Sc. from MIT. Paulo’s research interests range from behavioral operations management to sustainability and from diffusion of epidemics to humanitarian logistics. He was actively involved in modeling the diffusion of COVID19 and identifying effective policies to prevent its spread, working with authorities in both Canton Ticino, Switzerland, and East of England, UK. His recent research focuses on overcoming sustainability challenges, particularly leveraging policy synergies and mitigating policy tradeoffs to achieve the sustainable development goals (SDGs). He is former president of the System Dynamics Society (SDS), senior editor of POM and SDR journals, Intel Foundation Graduate Research Fellowship awardee, and the 2004 Council of Supply Chain Management Professionals (CSCMP) Doctoral dissertation awar
Judge Business School (CJBS). Prior to USI, He was visiting Assistant Professor at MIT Sloan and Assistant Professor at the University of Miami Graduate School of Business. Paulo holds a Ph.D. in Management Science and System Dynamics from MIT Sloan and a M.Sc. from MIT. Paulo’s research interests range from behavioral operations management to sustainability and from diffusion of epidemics to humanitarian logistics. He was actively involved in modeling the diffusion of COVID19 and identifying effective policies to prevent its spread, working with authorities in both Canton Ticino, Switzerland, and East of England, UK. His recent research focuses on overcoming sustainability challenges, particularly leveraging policy synergies and mitigating policy tradeoffs to achieve the sustainable development goals (SDGs). He is former president of the System Dynamics Society (SDS), senior editor of POM and SDR journals, Intel Foundation Graduate Research Fellowship awardee, and the 2004 Council of Supply Chain Management Professionals (CSCMP) Doctoral dissertation awar
The workshop will be held at the Koç University campus in Sarıyer, Istanbul.
Please feel free to contact the organizing committee if you have any questions.
We hope to see you at the workshop!
Organizing Committee
-
- Evrim Didem Güneş (egunes@ku.edu.tr),
-
- Özge Karanfil (okaranfil@ku.edu.tr )
-
- Lerzan Örmeci (lormeci@ku.edu.tr
*The 9th Annual Koç University Healthcare Operations Workshop is supported by the 2232 International Fellowship for Outstanding Researchers Program of TUBITAK..